As you know, colorectal cancer is the third most common solid organ cancer in adults, affecting men and women of all races equally. When detected early, it is highly treatable and, with proper screening, can even be prevented in many cases.
However, occasionally patients do present with advanced disease. It is in these instances that the expertise of a care team and the breadth of treatment options available become not just assurances, but necessities that can make the difference between life and death. As one of central Virginia’s primary referral centers for patients with colorectal cancer, UVA Cancer Center regularly treats complex colorectal cancer patients, and has been doing so for more than 20 years.
“We get referrals from all over the state, so our volumes for rectal cancer in particular are high, with about 50 surgeries performed every year,” says Chief of Colorectal Surgery Charles Friel, MD. “When it comes to this type of complex procedure, expertise and volume do matter. At UVA we are fortunate to have two experienced colorectal surgeons including myself and Dr. Traci Hedrick.”
Below is one case study that highlights the benefits of having not only a skilled team of colorectal surgeons, but also an army of experienced providers from multiple disciplines collaborating to deliver advanced care to one patient with complex medical needs.
Case Study: Stage IV Colorectal Cancer with Perforated Bowel and Spinal Infection
Patient: Michael Miller, age 43
Assessed by:
Frank Shen, MD, Spine Surgery
Charles Friel, MD, Colorectal Surgery
Tri Minh Le, MD, Oncology
Kelli Reardon, MD, Radiation Oncology
Victor Zaydfudim, MD, Hepatobiliary Surgery
Presented with: Fever, weakness, back and neck pain
“It all started with fever and chills, but it always went away so I ignored it,” says Miller. “Then my back started hurting. I went to a chiropractor, which helped initially. Then about a week later, I collapsed on the living room floor because the back pain was so severe.” Once admitted to UVA Emergency Department, an evaluation revealed that Miller had an extensive spinal abscess and a pelvic abscess that appeared to be the source of E. coli bacteremia.
Diagnosis: Sepsis
“The initial diagnosis was unclear,” says Friel. “We knew he had sepsis that had spread to his spinal column. This became the immediate problem.”
Sepsis Treatment: Multi-level decompression laminectomy
“[Our care team] came together to discuss the possibility of treating the infection with percutaneous drainage and antibiotics, but the infection was too severe,” says UVA Orthopedic Spine Service Division Head Frank Shen, MD. “When I first saw him, he looked like someone preparing to die. His body was trying to fight off a severe infection; he was hypotensive, his white count was elevated; he was extremely weak and was essentially becoming paralyzed. Without treatment, the next likely step would have been death. I had no choice but to take him into surgery.
“What was particularly challenging and extremely unusual about Mr. Miller’s case was the extent of his spinal infection,” adds Shen. “Ordinarily, infections like this are limited to smaller segments of the spine. In these cases, we would remove bone and ligament and then replace it with rods and screws. However, in this case, the infection was in the entire spine, from the base of the skull to the tailbone. It was wrapped around the spinal cord and nerves, so I had to surgically drain the infection while trying to preserve as much ligament and bone as possible to avoid the need for fusion and stabilization with rods and screws. These can make it harder to clear the infection and, in Mr. Miller’s case, would have led to complete loss of all spinal motion.”
As a result, Shen performed a more technically challenging procedure called skipped laminectomies, during which he removed portions of bone and ligament from every other vertebra, from the base of the skull down to the tailbone, to reduce compression and irrigate the extensive infection, while preserving stability. A few days later, this procedure was repeated again to help eliminate any remaining infection in Miller’s spine.
After the spine surgery, Miller was unable to move. “I was in the ICU for about a week and a half. I was completely paralyzed,” says Miller. “It was quite a shock to wake up and be reliant on others to feed me — as an adult, that’s difficult.”
Miller was treated with long-term antibiotics and was transferred to HealthSouth for inpatient rehabilitation to regain his strength. “When I saw him four weeks after surgery, he was still limited in his mobility and used a wheelchair,” says Shen.
Diagnosis: Stage IV rectal cancer with metastases to the liver
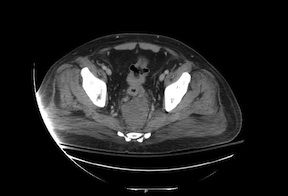
An extensive evaluation, including an endoscopy and CT imaging, revealed that the cause for Miller’s life-threatening spinal infection was perforated rectal cancer. Complete cancer staging demonstrated stage IV rectal cancer with liver metastases. “His tumor had perforated, causing an abscess,” says Friel. “It was also partially obstructing, so he needed a colostomy to divert his stool.”
Treatment: Fecal diversion, systemic chemotherapy, chemoradiation, tumor resection
Friel performed a colostomy to allow Miller to relieve his obstruction. “We had to get over the immediate situation, then our entire team could get together to come up with an individualized, sophisticated care plan designed to treat him and make every attempt to cure him,” says Friel.
After recovery from infectious complications and the colostomy, Miller began systemic therapy with a combination of three-drug chemotherapy, with the addition of targeted monoclonal antibody regimen. “After six total cycles of chemotherapy, re-staging CT scans showed significant disease response and the decision was made to continue with six additional cycles in light of his good treatment tolerance,” says oncologist Tri Minh Le, MD. “After extensive discussion at our multidisciplinary tumor board, the decision was made to pursue surgical resection of his remaining tumor burden following chemoradiation to the primary tumor site.”
In combination, chemotherapy and external beam radiation to the rectum allowed for both systemic and local tumor control.
Approximately 11 months after Miller’s initial presentation, Friel and hepatobiliary surgeon Victor Zaydfudim, MD, performed a combined procedure to remove the rectal cancer and liver metastasis. Friel also reversed the colostomy and constructed a temporary ileostomy.
Outcome: Almost complete recovery from infectious complications and no evidence of cancer recurrence
At a follow-up in early December, Miller was doing well. “He has some very small ‘spots’ on his lungs that we are watching carefully,” says Friel. “We are cautiously optimistic at this time. He will have his ileostomy reversed in a few weeks. Overall, he looks great.”
“I take it day to day,” says Miller. “I have some numbness and tingling in my fingers, but I am able to walk up the stairs with a cane. I may never be 100 percent again but I hope to be as close to normal as I can.
“There were a lot of people involved in my care along the way. From the top surgeons to the people who brought me my food tray — it’s clear they are dedicated to excellent patient care. That’s what UVA is all about.”
“In the past, a case like this would have been hopeless,” adds Friel. “Now with advanced surgical techniques, new chemotherapy agents and the high level of expertise that comes from a multidisciplinary approach to care, we can explore all options to treat Stage IV disease.”
To learn more about the treatment of colorectal cancer at UVA, including clinical trials now enrolling, go to uvahealth.com.
To arrange an on-site visit with one of the providers mentioned above, please contact our Physician Relations team.