At a Glance
- A dural arteriovenous fistula (dAVF) can pose a high risk of spontaneous bleeding.
- Most dAVFs can be treated by endovascular transarterial embolization.
- In a recent case, direct access to the dAVF was blocked, so UVA neurosurgeons took advantage of the capabilities of the hybrid OR/angiography suite to modify their approach and successfully embolize the dAVF.
- The hybrid OR gave neurosurgeons the option of open surgical resection if the embolization was unsuccessful.
In 2015, UVA was the second medical center in the country to open a neurovascular operating room suite equipped with intraoperative MRI and biplane angiography. The benefits: MRI and angiography provide an extra level of precision and control, allowing neurovascular surgeons to monitor the patient in real time. Angiography, in particular, is valuable for visualizing blood vessels during microsurgery.
The hybrid OR also gives UVA neurovascular surgeons unusual flexibility in addressing rare or difficult-to-treat conditions. In the hybrid OR, neurovascular surgeons can choose among minimally invasive, endovascular and traditional open procedures or even combine them as treatment demands.
“Very few centers have the facilities to perform this type of combined open surgical and endovascular procedure,” says neurosurgeon Min Park, MD. “We are fortunate at UVA in having the equipment and resources to conduct it.”
Equally important, UVA has specifically recruited neurosurgeons with expertise in both endovascular and open surgical approaches. Park completed a fellowship in endovascular neurosurgery and has a vast knowledge of neurological disease, which allows him to provide patients the most appropriate treatment options for their conditions.
The advantages of having a hybrid OR and a highly trained team of surgeons are clearly evident in the case study below, highlighting one patient whose dural arteriovenous fistula (dAVF) could not be completely embolized using standard endovascular embolization.
Case Study: Dural Arteriovenous Fistula
Patient: 45-year-old man
Assessed by: Team led by Min Park, MD
Presentation: During routine MRI surveillance following treatment for melanoma, the patient’s oncologist noted abnormal vascularity at the left temporal occipital junction. The patient reported having experienced intermittent pulsatile tinnitus during the previous months.
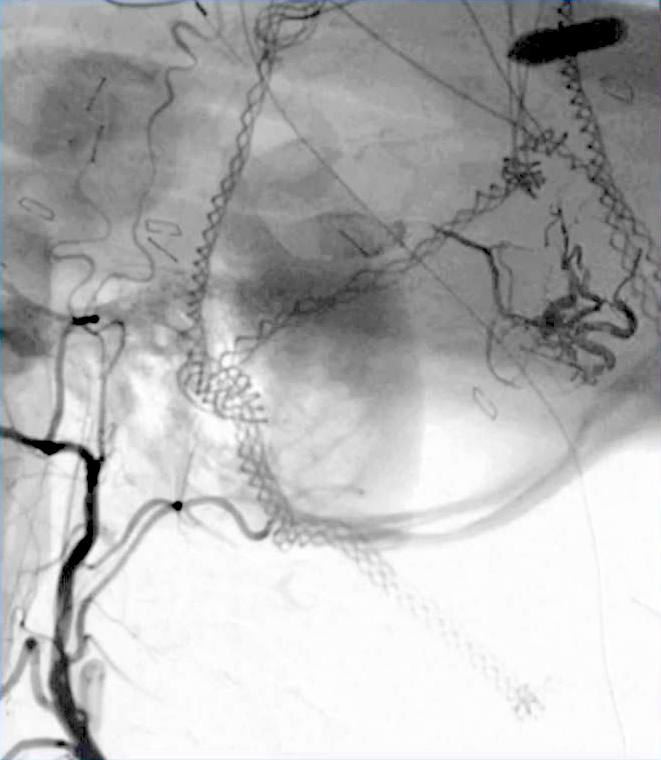
Diagnosis: An angiogram demonstrated that the patient had acquired a high-risk dural arteriovenous fistula fed primarily by the left middle meningeal artery (MMA), as well as branches of an enlarged occipital artery.
Treatment: The UVA neurosurgical team performed a partial endovascular embolization of the portion of the fistula served by the left occipital artery, but was unable to navigate a portion of the middle meningeal artery with a microcatheter.
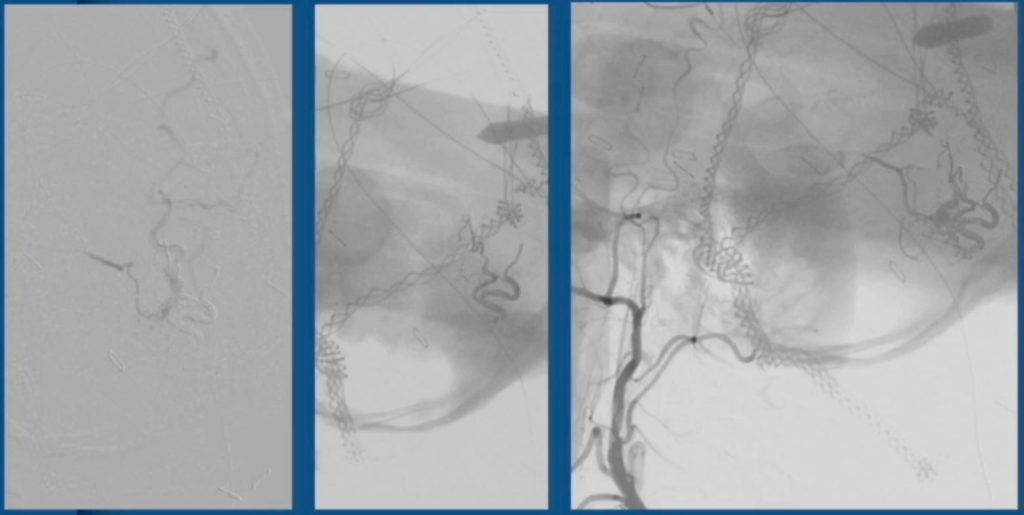
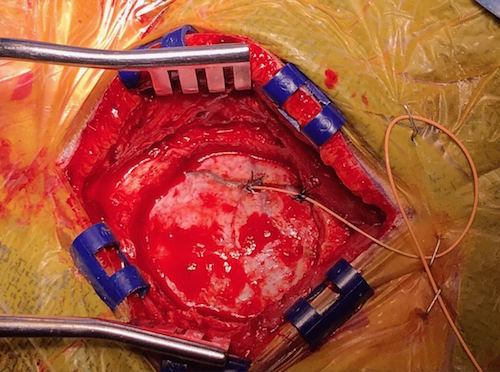
A month later, they brought the patient into the hybrid OR and performed a small targeted craniotomy that provided access to the MMA at a point between the tortuous segment and the dAVF. The team then positioned the microcatheter in the MMA, secured it in place and completed the embolization.
“Being able to access angiography was beneficial in a number of ways,” Park says. “It enabled us to position the craniotomy with a high degree of precision, which allowed us to make it as small as possible. We also used it to confirm the placement of the microcatheter in the MMA — all in addition to enabling us to complete the embolization.”
Recovery: The patient was discharged the second day after surgery and had a follow-up angiogram six months later.
Outcome: The patient’s dAVF has been completely and permanently eliminated. Post-embolization imaging reveals no filling of the fistula and no venous drainage.
“Because of the connections between the arteries and the dural sinuses, traditional open surgery can be difficult,” Park says. “Having the facilities to pursue this hybrid approach was invaluable.”
To refer a patient to UVA Health System, call UVA Physician Direct at 800.552.3723.