The move to less invasive procedures has impacted all areas of medicine over the past 15 years, according to Gilbert R. Upchurch, Jr. MD, Division Chief, Vascular and Endovascular Surgery at University of Virginia Health System. When it comes to treating stenosis of the carotid artery, this means a shift from carotid endarterectomy (CEA) to carotid stenting in certain patients.
“UVA has been performing carotid stenting since the 1990s and has been involved in many of the important clinical trials to determine who should get the stenting procedure,” says Upchurch. The most significant, CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) was an NIH-sponsored study that compared the two procedures and found stenting to be just as effective as CEA.
Interventional radiologist Avery Evans, MD, was the principal investigator for the CREST study at UVA, one of 100 centers nationwide that participated. “Stenting is now mature technology proven safe and effective,” says Evans.
Best Candidates for Carotid Stenting
According to Evans, patients who have the best outcomes with the less-invasive approach include those who have had prior surgeries or radiation to the head and neck, which causes the formation of scar tissue; patients who are at an average or high risk for traditional surgery, including those with pulmonary problems who may suffer complications from anesthesia; as well as patients who are relatively younger. By pinpointing the best candidates, stenting has resulted in more positive outcomes.
Procedure Overview
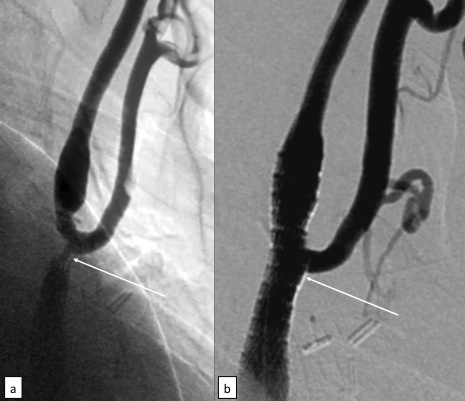
Because this procedure causes limited pain and discomfort, light sedation is used instead of general anesthesia. After the patient is sedated, a sheath is inserted into the femoral artery and a catheter is threaded through the sheath up to the carotid artery.
A distal protection device, or filter, is then inserted above the point of stenosis. This filter catches any debris that may detach during the procedure and prevents it from traveling through the carotid to the brain, which can lead to stroke. Once the filter is securely in place, a surgeon inserts a balloon-tipped catheter and runs it to the area of the carotid artery that is blocked or narrowed. The balloon is inflated, pushing the plaque to the artery walls and opening the artery. A small stent is then inserted to keep the artery open and maintain adequate blood flow.
Once the artery is open, the distal protection device is collapsed to securely hold any debris and retracted. Postprocedure, patients are monitored in the ICU overnight and receive an ultrasound to ensure blood is flowing adequately through the carotid artery postprocedure.
Risks Associated with Carotid Stenting
There are risks associated with both CEA and stenting. The incidence of stroke is higher with stenting, and heart attack rates are higher with surgery, according to study results presented at the American Stroke Association International Conference in 2010. According to Upchurch, less invasive is typically better, especially in some high-risk patient groups. “The overall impact on the body is greater with surgery,” he says.
At UVA, there are two interventional cardiologists as well as two endovascular neurosurgeons who perform carotid stenting procedures. To find out if your patient may be a candidate for carotid stenting or to discuss other endovascular treatment options, email Avery Evans at AJE5U@virginia.edu.