UVA Health cardiovascular researchers have developed new MRI techniques that allow them to see what other heart tests can’t: the makeup of the fat surrounding the heart, and how it may be silently fueling heart failure.
“What we found is that the more saturated fatty acids you have in the fat around the heart, the more pro-inflammatory the fat becomes,” explains UVA cardiologist Amit Patel, MD. “That inflammation then gets released straight into the heart muscle.”
The result? A constant stream of inflammatory signals that flows into the heart and sets the stage for heart disease.
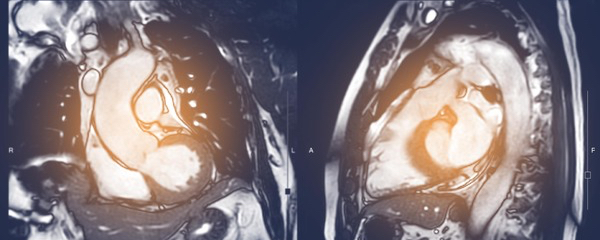
An MRI That Sees Inside Epicardial Fat
The fat that hugs the outside of the heart, called epicardial adipose tissue (EAT), may become inflamed and affect the heart muscle under certain disease conditions.
Until now, there hasn’t been a way to accurately measure what’s happening inside EAT. Patel and his collaborators at UVA and UVA Health, in particular Fred Epstein, PhD, and his team, changed that by developing high-speed MRI techniques that can identify the chemical makeup of EAT in terms of the ratios of saturated, unsaturated, and polyunsaturated fatty acids.
Other groups have looked at fat composition before, but only in other areas of the body. “People had done fatty acid composition imaging in the abdomen, but the abdomen doesn’t move,” Patel says. “They didn’t have to worry about the speed. What Fred Epstein and his team did here is figure out the speed problem.”
The heart and thoracic cavity are constantly in motion, with the heart beating and lungs expanding and deflating. And the accuracy of MRI scans is degraded by motion. This presented a major engineering challenge.
When measured in the MRI scanner, molecularly, “different fatty acids spin at slightly different frequencies,” Patel explains. “So they had to develop MRI techniques that could collect data fast enough to capture those differences — all within 10 seconds, while the patient holds their breath, and only when the heart is perfectly still. Their innovation was to develop an MRI technique where they could collect the data so fast that it could actually differentiate between these spins.”
The team captured data during those short windows of stillness when neither the heart nor lungs are moving. They relied on cutting-edge acceleration and undersampling techniques to gather enough usable data.
“In order to differentiate the spins, the only way they could do that is by not collecting too much data — collect it very quickly and very sparsely,” explains Patel. Then, “they applied advanced mathematical modeling and simulations to fill in all the missing data mathematically.” The software automatically analyzes the raw MRI data and presents a color-coded image of the fat composition.
The result is the only known current MRI method to assess fat composition in the beating human heart.
Patterns in Fat Composition & Heart Functions
Epstein, Patel, and the team tested their approach in healthy volunteers and in 21 patients who had recently experienced ST-segment elevation myocardial infarction (STEMI). All patients underwent cardiac MRI within 96 hours of reperfusion. Alongside fatty acid composition imaging, participants also had standard assessments of left ventricular (LV) structure and function, infarct size, and EAT volume.
In these STEMI patients, the researchers found that EAT had a significantly different fatty acid profile compared to other areas of fat, like visceral and subcutaneous fat. EAT had lower levels of polyunsaturated fatty acids and higher levels of monounsaturated and saturated fatty acids. These differences in fat composition appeared to be linked with changes in the heart’s size, mass, and pumping action.
Particularly, higher levels of saturated fat in the EAT were associated with larger left ventricular volumes and mass, and a trend toward reduced ejection fraction. These changes were not explained by infarct size alone. This suggests that EAT composition may provide independent insight into how the heart responds after a heart attack.
Translating Innovations to the Clinic
As Patel and the team continue enrolling patients, they hope to uncover more connections between fat, inflammation, and heart disease to drive individualized care.
“Theoretically, since there is no contrast agent, since there is no radiation, fatty acid composition could be used as a screening test one day,” says Patel. “You could look at a person with risk factors and say, ‘Wow, you have a lot of saturated fatty acids there. Maybe you need to change your diet and exercise, and see how it changes.'"
Patel credits the success of the project to UVA’s close collaboration between cardiology, biomedical engineering, and computer science. “The reason I came here, moved to Charlottesville, is literally because of the ability to work with biomedical engineers and computer scientists,” he says. “Translating new development to help care for a patient and answer unknown questions with new technology — for me, that’s very exciting.”