At a Glance
- Millions of women are living with the symptoms of overactive bladder.
- When medication and conservative therapies are ineffective, physicians should consider referring women to UVA to be evaluated for Botox therapy.
- UVA is utilizing a new approach to Botox therapy, using fewer injection sites.
- UVA is also administering antibiotics prior to treatment to reduce the incidence of UTIs.
As many as 40 percent of women in the U.S. live with the symptoms of overactive bladder (OAB), according to the Urology Care Foundation. However, that estimate only includes those who report their symptoms — the true count is likely much higher.
That means millions of women are living with often-embarrassing symptoms that can greatly impact quality of life, including:
- Frequent urination or urge to urinate
- Urge incontinence
- Nocturia
First-line therapies – behavioral modifications and anticholinergic medications (oxybutyinin, tolterodine and solifenacin) – are effective for some women. However, for those who don’t respond to conservative therapies or medication, Botox® has become a viable option.
“Providers should consider referring patients with OAB to a urogynecologist sooner rather than later,” says UVA urogynecologist Monique Vaughan, MD. “After a patient has failed conservative therapy and had no results with one medication, then it’s a good idea to start the conversation about Botox therapy so they can be screened for eligibility.”
Who’s Eligible
“There are two types of patients that this therapy greatly benefits," says urogynecologist Elisa Trowbridge, MD, division director for UVA Female Pelvic Medicine and Reconstructive Surgery. These include:
- People who have failed multiple medications for OAB
- Those who have urinary urgency and frequency (>10 voids/day), as well as urinary leakage associated with urgency.
“These are women who have to go to the bathroom all the time, day and night, and nothing works for them,” says Trowbridge. For patients like these, she says, Botox has been “a game changer.”
Patients who are not good candidates for Botox treatment are those with chronic urinary tract infections and those who have trouble with incomplete emptying of the bladder.
How it Works: Now Vs. Then
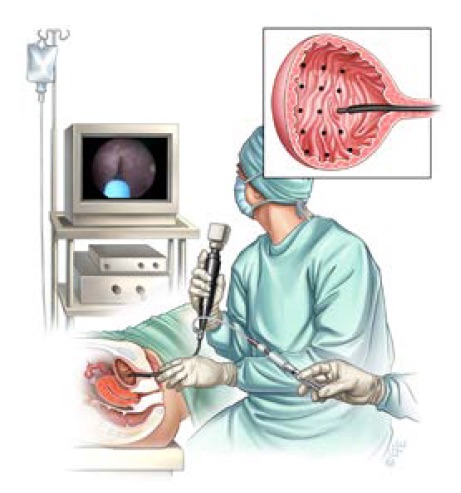
The Botox procedure for OAB is performed primarily in the clinic setting, but may also be performed in an ambulatory surgical center under mild sedation.
It takes about ten minutes to complete. Doctors perform a cystoscopy and partially fill the bladder with saline. In the past, the doctor would then administer about 10 to 15 injections into the dome of the bladder. Today, UVA providers have cut the number of injections in half.
“We’re still using the same amount of medication, but we’re doing fewer injection sites –- around five,” says Vaughan. “A recent study showed that this approach is just as effective at decreasing the number of incontinence episodes compared to the traditional 10 to 15 injection sites. But with fewer injection sites, patients tolerate the procedure better because there is less discomfort.”
Another change UVA has implemented is administering antibiotics sooner to lower the risk of urinary tract infection post-procedure, which affects around 20% of patients. “I coauthored a paper published recently that showed it was beneficial to start antibiotics before administering Botox injections compared to starting them after,” says Vaughan. “Those patients who received antibiotics before the procedure had a decreased frequency of UTIs. So that is what we are doing currently at UVA.”
Botox typically loses its effect after about six to nine months, so the procedure is typically performed twice a year as necessary. Medicare and other major insurers cover Botox as a treatment for overactive bladder if medication and behavioral therapy have been ineffective.
An Effective Alternative
Compared to other options, results from the Botox treatment are impressive. “In 10 minutes, around a third of patients are completely cured,” says Trowbridge. “Sixty percent have a 50% reduction in the number of accidents they have. And again, you’re doing all this with next to no complications or side effects. It’s a great option for patients who have suffered for so long.”
Print this flyer to share with patients you feel may be candidates for Botox treatment.
To refer a patient to UVA Female Pelvic Medicine and Reconstructive Surgery, call 800.552.3723. To speak with the clinic directly, call 434.924.2103.