From reduced recovery time to lower infection risk, minimally invasive procedures bring significant benefits for patients. At UVA Health, we’re driving this trend forward in gastroenterology.
Gastroenterologist Andrew Wang, MD, Division Chief of Gastroenterology and Hepatology and Director of Interventional Endoscopy, helped pioneer “third-space” endoscopy in the U.S., bringing this alternative to invasive surgery to treat patients with conditions ranging from GI cancer to achalasia.
Wang has collaborated with other experts to publish two Clinical Practice Updates in this area. He shares his insights.
While the first space is on the inside of the gastrointestinal tract and the second space is outside of the organ in the chest or abdominal cavity, third-space endoscopy focuses on the space between the lumen and the outside wall of the GI tract.
“Third-space endoscopy has major advantages in two areas: First, as it pertains to treating early cancers while preserving the GI organ and second for patients with benign but severe conditions that affect esophageal or gastric motility,” says Wang. “It means providing a less-invasive option for patients with certain GI conditions that would otherwise require surgery.”
Organ-Sparing Cancer Treatment
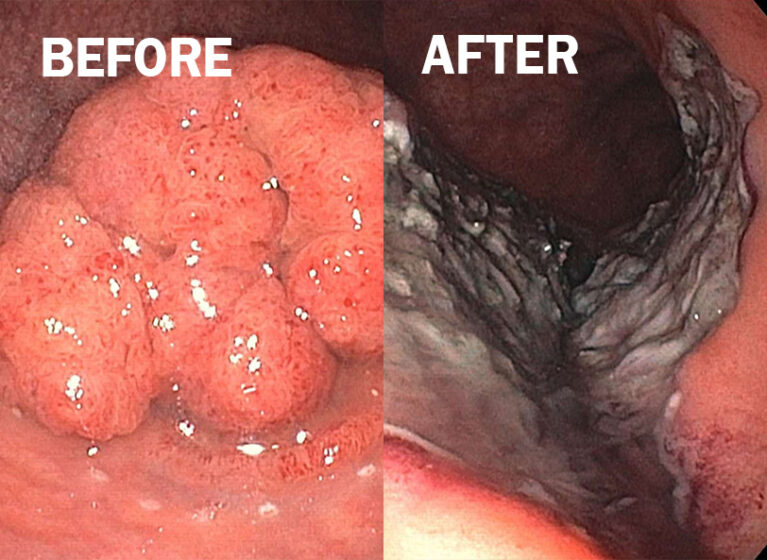
Using techniques learned from Japanese and Korean doctors, Wang brought endoscopic submucosal dissection (ESD) to UVA Health in 2010, making it one of the first facilities in the United States to offer the procedure. As a major shift in treatment approach, ESD is used to remove precancerous lesions or cure early cancers in the GI tract, including in the esophagus, stomach, colon, and rectum. During ESD, gastroenterologists work in the submucosal layer to cut out polyps and cancers arising from the mucosal layer while leaving the rest of the GI wall intact.
“Previously, if you had cancer, such as an esophageal or gastric adenocarcinoma, the surgeon would remove your esophagus or large parts of your stomach,” says Wang. “These surgeries significantly impact your quality of life. What ESD offers is an organ-preserving endoscopic procedure that allows patients to live normally and survive without surgery.”
Like Mohs surgery for skin cancer treatment, ESD spares significantly more healthy tissue than previous treatment options. Developed in Japan in the 1990s in response to the high rate of stomach cancer there, ESD proved to be a game-changer for treating these early cancers. By 2010, the endoscopic tools started to be available in the U.S. As an early adopter of this minimally invasive endoscopic technique, Wang has been a national leader in this area. Over the past decade, the procedure has become easier to perform due to better tools and advancements in procedural techniques. ESD benefits patients who might not be surgical candidates, including frail and elderly patients.
“These procedures have improved patients’ lives by offering an alternative to more invasive surgery,” says Wang. “During ESD, the submucosal space becomes a working space where we can cure cancers arising in the mucosa that might invade into the submucosa by removing all the cancerous or precancerous tissue in one piece, which allows accurate pathological diagnosis and spares otherwise healthy tissue.”
Wang led a group of experts who recently published an American Gastroenterological Association (AGA) Institute Clinical Practice Update on surveillance in patients with cancer or precancerous lesions treated using ESD. With this focus, Wang and colleagues from around the country are conducting research to help patients and further the emerging field of endoscopic oncology. The goal is to ensure that patients get optimal outcomes.
Alternative to Heller Myotomy Surgery
After Wang and his team gained experience in ESD, they expanded their work in the third space to other procedures, including, in 2014, esophageal per oral endoscopic myotomy (POEM) to treat swallowing disorders, such as achalasia. Wang was the first gastroenterologist in Virginia to provide this procedure to help patients with achalasia be able to eat again.
“What we were able to do as an extension of third-space endoscopy was make what used to be invasive Heller myotomy surgery an elegant endoscopic procedure,” says Wang. “We can now tunnel into the wall of the esophagus with a scope. With this procedure, there are no laparoscopic incisions in the abdomen, which would be required for surgery.”
The POEM technique has become a gold standard third-space endoscopic procedure and has expanded from the esophagus down the GI tract into the stomach. Within the last three years, UVA Health has used POEM to open the pylorus — which is the muscular outlet of the stomach — in patients with severe gastroparesis, which can be due to diabetes or may occur as a consequence of a heart or lung transplant. Most recently, Wang was part of a group that published a separate AGA Clinical Practice Update on using gastric POEM to treat medically refractory gastroparesis.
“If you can spare an organ, you can help preserve that person’s lifestyle,” says Wang. “Esophageal and stomach surgeries can be high-risk procedures, and patients’ lives are different afterwards. With POEM, we can offer outcomes as good as surgery for patients with achalasia.”
Wang and his team have also leveraged third-space endoscopy techniques to treat patients with symptoms from a Zenker’s diverticulum. Wang has taught physicians at UVA Health and has worked for many years to share this procedural knowledge with other talented physicians across the country. As POEM and ESD have become mature procedures with good published outcomes, UVA Health has continued to lead and educate in this area, making these techniques more accessible.
Bringing a Different Approach to Tumor Boards
In the future, Wang recognizes that endoscopic procedures will become less relied upon for diagnosis of clinical problems as biomarkers, blood- and stool-based tests, and even artificial intelligence improve. However, he is certain that therapeutic endoscopy is here to stay, and its applications are sure to grow in treating patients with GI illnesses. What the team has achieved at UVA Health in the third space and in advanced endoscopy is only the beginning in what should be an exciting future where patient care will become more precise and tailored, with enhanced outcomes.
“At UVA Health, we bring a team approach as we work with surgeons, oncologists, radiologists and pathologists at our multidisciplinary tumor boards,” says Wang. “We have really great collaboration, which means the right patients get directed to the right procedures with the best outcomes. We’re not replacing surgery but sparing those who don’t need it, and we are trying to assure patients who require more radical surgery that they are making the best choice. That’s what we are all about.”
UVA Health has been an optimal proving ground for these innovative procedures, especially given the institution’s expertise in treating patients with benign and malignant conditions of the GI tract.
“Because of our experience, we have been a referral center for these procedures for a long time,” says Wang. “We want to share knowledge on how working in the third space can cure some patients with early cancers by offering a minimally invasive, scarless endoscopic procedure.”
Still, Wang says, it’s not enough to just treat patients at UVA Health, and there needs to be a renewed focus on education and research in the field of advanced endoscopy and endoscopic oncology: “We are proud to offer these procedures at UVA Health, and we hope to contribute to the knowledge and understanding in the field so that outcomes can be optimal for patients everywhere.”