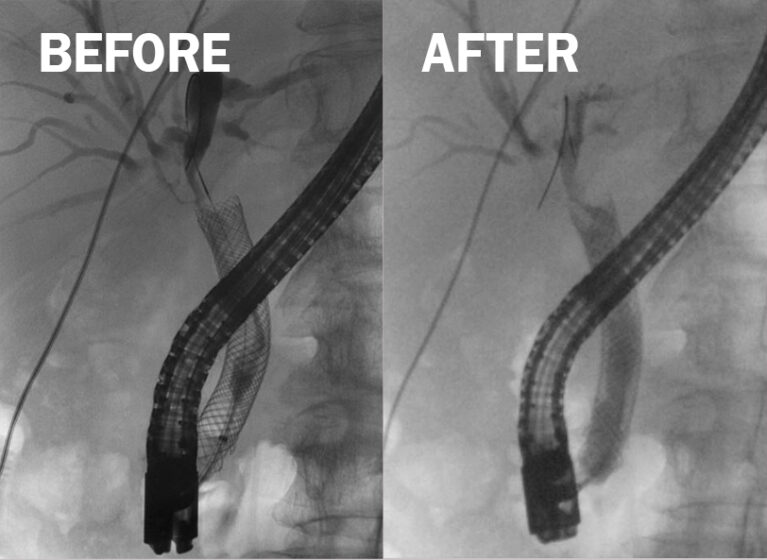
Biliary tree during an ERCP before and after RFA
Endobiliary ablation procedures performed at UVA Health offer hope for patients with cholangiocarcinoma and pancreatic cancers.
The nonsurgical procedures improve survival rates for people with incurable cholangiocarcinoma or pancreatic cancer and help control symptoms of the condition in patients waiting for a liver transplant, says Ross Buerlein, MD, gastroenterologist and hepatologist.
As a national and international leader in endobiliary ablation, UVA Health continues to research ways to advance the use of endoscopic retrograde cholangiopancreatography (ERCP)-directed radiofrequency ablation (RFA) and photodynamic therapy (PDT) to improve patient care.
Enhancing ERCP to Extend Survival
Cholangiocarcinoma and pancreatic cancers are often considered unresectable at the time of diagnosis due to the cancer’s stage, location, or size, Buerlein says.
Traditional ERCP helps keep bile ducts open, but does not impact survival.
“We wanted to see what we could do to improve patient survival while keeping bile ducts open longer,” Buerlein says.
He and colleagues started studying endobiliary ablation methods a decade ago.
When combined with traditional ERCP, radiofrequency ablation or photodynamic therapy can be deployed at cancer sites within the bile ducts, destroying cancerous tissue. By removing cancerous growths — some of which cause narrowing ducts even with stent placement — the bile ducts stay open longer.
“It’s important to consider this when thinking about all the options available to the patients,” Buerlein says.
For example, in the past two years, a new immunotherapy drug called durvalumab became available. When combined with standard chemotherapy to treat cholangiocarcinoma, the patient survival rate improved by six weeks.
The news made waves and was considered a breakthrough. However, the therapy costs more than $100,000 for one year, Buerlein says.
Radiofrequency ablation or photodynamic therapy on average doubles survival compared to durvalumab and costs much less, Buerlein says. “If a patient is already undergoing an ERCP for blocked bile ducts, doing the ablation just makes sense.”
UVA Health combined its data with that from other institutions during the past 10 years to assess the efficacy of endobiliary ablation. The results show improvement. Notably, patients who receive endobiliary ablation versus stenting alone survive three months longer.
Optimizing Care for the Future
Endobiliary ablation is sure to evolve in the future. UVA Health physician-scientists will study ways to optimize the procedures. Plans call for studying whether radiofrequency ablation or photodynamic therapy performs better under different circumstances, such as the:
- Amount of time a stent can be left in place
- Best number of sections to treat at one time
- Location of the cancer
- Number of times the treatment can be used in the same location
- Optimal amount of electrical energy to use during ablation
“There are nuances we might be able to optimize, and we need to look at those in our research,” Buerlein says.
Buerlein and colleagues also hope to spread the word about endobiliary ablation. UVA Health’s endoscopy fellows are one avenue for accomplishing that. These doctors are trained in the procedures while studying at UVA Health. Many now work across the United States and Canada.
Oncologists and cancer surgeons at UVA Health consult with Buerlein and others on the gastroenterology and hepatology team when they are managing a patient with surgically unresectable cancer.
“Despite data supporting the use and safety of endobiliary ablation and its improvement of survival rates, it is not well known or discussed frequently among outside interventional endoscopists or oncologists,” Buerlein says.